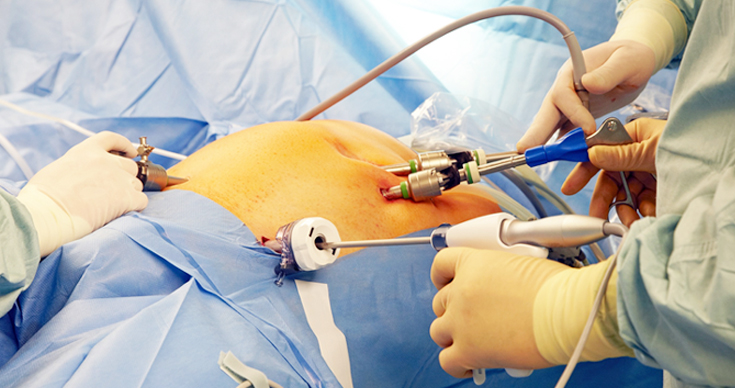
Everything You Should Know About Minimally Invasive Surgery or Most commonly known as Key-Hole Surgery/Laparoscopic Surgery
Minimally invasive surgery which is most commonly known as the Key-Hole Surgery or Laparoscopic Surgery, is a specialised and advanced technique for conducting surgeries. This has been a popular technique for gynaecological procedures as well as gallbladder surgery. Laparoscopic surgery is one of the common types of minimally invasive surgeries, conducted by making small incisions, using tiny cameras, small tubes and surgical instruments. Constant innovations in the industry has led to these surgeries being shorter, with a faster recovery time, less invasive and painful along with fewer complications.
Scope of Key-hole Surgery / Minimally Invasive Surgery

Key-hole Surgery / Laparoscopic Surgery has been a popular choice for gynaecological procedures and gallbladder surgery. However, over the years, the scope for this key-hole surgery / minimally invasive surgery has increased to cater to many other surgical procedures. Now there’s scope for laparoscopic surgery for small and large intestinal surgeries, hernia repair, treatment for infertility. It is also used for diagnostic purposes like knowing the stages of cancer, checking for tumours or evaluation of the effectiveness of some treatment.
Advantages of Key-Hole Surgery / Minimally Invasive Surgery
In traditional open surgery, the doctor makes a large cut for visibility of organs and then operates on the patient. In case of minimally invasive surgery, here are some advantages that make it a better choice over traditional surgery:

- The surgeon can limit the number of cuts, the size of the incisions made and is considered much safer than traditional open surger
- The recovery period after a minimally invasive surgery is faster with smaller incisions leading to tiny or negligent scarring
- Not a lot of muscle or skin is opened up or affected, especially in key-hole surgery. The robotic surgeries are done with extreme precision
- The chances of complications also reduce in case of minimally invasive surgery, be it laparoscopic surgery or minimally invasive surgery
Along with the benefits, there is scope for major innovation and betterment of the current procedures, which is being worked on every minute by various surgeons all over the world. Minimally invasive surgery makes it easier for the patient and as well as the doctors and is the best solution to your issues. ILS Hospitals being the pioneers in laparoscopic surgery has been a leading hospital in Kolkata with renowned surgeons and facilities for key-hole surgery or minimally invasive surgery. To consult or know more about minimally invasive surgery, visit www.ilshospitals.com.
Make Faster Recovery And Wear Anything Confidently After Minimally Invasive Gynecological Surgery
Being a woman is hard in many aspects. You go through many phases in life and nurture not only yourself but also the lives of your loved ones. But when it comes to your health, many women are not even aware or concerned about it unless it becomes too severe. Many illnesses loom over women, particularly that require gynecological surgery. Many gynecologists in Kolkata often find that a lot of women do not prefer to undergo surgery and look for oral medicinal treatment instead even if a surgery is vital for them. There are 2 main reasons for the same, they assume –
- It will be painful and need much recovery time and they will not be able to fulfill their duties in personal and professional lives.
- It will leave big scares in their abdominal or pelvic region and thereby will make it look unattractive.
Today we will focus on the Minimally Invasive Gynecological Surgery (MIGS) and how it overcomes the Drawbacks of Open Surgery.
Gynecological surgery implies surgical treatment of the organs in the female reproductive system. It is done to address problems like uterine inconsistency, infertility, removing tumors (both benign and malignant) and carry out procedures like hysterectomy or tubal ligation.
Earlier all these procedures were carried out by making a large incision across the abdomen or pelvic region. It used to leave large scares throughout life. Though certain medication can help the stitch marks to fade over time, it still remains distinguishable and thus, many women feel embarrassed to wear sarees and lehengas after surgery.
Modern medical science has the perfect solution for the same, in the form of minimally invasive gynecological surgery. These surgeries are carried out through a few minute incisions made near the abdomen. Some special equipment, camera, and light sources are inserted inside the abdominal or pelvic cavity and the doctor carries out the surgery through the same. Once the procedure is over, the incisions are closed using stitches.
As the surgery does not expose the internal organs, it offers multiple advantages, such as
- Lesser risks of operation such as bleeding, infection, injury to the nearby organs
- Much lesser need for blood transfusion (almost nill)
- Lesser risks after the operation such as swelling and infection of the surgical site
- Less painful
- Early discharge from the hospital
- Faster recovery
- Much early resuming to daily life works
- Better aesthetic look of the abdominal/pelvic region as the procedure is almost scarless
So, in case you too are looking forward to having any gynecological surgery, come at ILS Hospitals, as we offer MIGS for a wide range of gynecological procedure.
For more information visit us now!
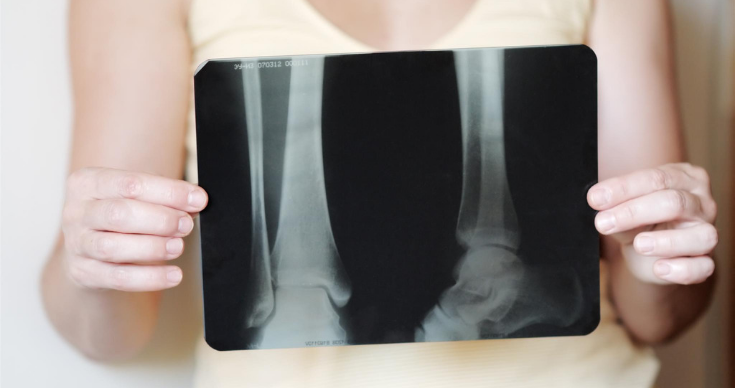
Why Women Are More Prone To Osteoporosis
There are many factors that make an individual susceptible to any particular disease. Often such factors can be smoking, drinking alcohol, aging, having some underlying illness and so on. As per many orthopedic experts, women are more susceptible than men, when it comes to osteoporosis. Let’s find out the reasons why women are more likely to have osteoporosis than men.
Osteoporosis is an orthopedic condition in which the bone becomes porous. As a result, eventually, it leads towards making them weak and brittle. It can easily lead to a fracture even due minor to mild trauma or accident.
There are mainly 2 reasons for women being more susceptible to have osteoporosis.
Bone Structure
Osteoporosis often happens due to certain factors that are prominent during childhood and adolescence. Women reach their peak of bone mass growth around age 18, for men it continues to grow around the age of 20. Moreover, women have smaller bone structure as compared to men, as a result, their bone mass density is lower than that of men. These factors make women more susceptible to have orthopedic conditions.
Role Of Estrogen
The female hormone, estrogen is the main reason for the likelihood of osteoporosis in women. Estrogen keeps the fertility cycles in check. Simultaneously, it also keeps the bones healthy and strong and things work well until the time of menopause. After menopause, the hormonal level drops significantly and act as a big factor to cause low bone density.
The reason being, women keep on losing bone density after menopause. In fact, as per gynecologists, women who have menopause at a younger age are at even more risk of the same. In contrast, women having their cycles at an earlier age or the ones using contraceptive (with estrogen) often have healthier bone mass.
Moreover, having irregular periods or start having them at a much later age are also some reasons for lower bone mass than others. Apart from these, having the ovaries removed can also cause lower bone mass.
Thus it can be concluded that women are at higher risk of developing osteoporosis and often other orthopedic conditions as well. As per studies, it has been found that one out of every 2 women above the age of 50 is likely to have osteoporosis. However, that does not mean, nothing can be done to address it. Regular exercise, intaking adequate vitamin D and calcium are highly beneficial to ensure a strong bone build-up. Osteoporosis is a disease that requires timely treatment to make sure it does not result in any severe complication.
At ILS Hospitals, we offer excellent orthopedic treatment and care for people who are enduring pain and discomfort for years. It’s time to address them effectively and lead a much healthier life ahead.
Common Gynecological Problems Faced by Women of Different Age Groups
Aging is a natural progression for both men and women and it helps them acquire new experience and expertise. However, it also brings new challenges to health-wise. Today, we are going to discuss what gynecological problems women go through, at different phases of life.
Gynecological Problems During Adolescence
1. Delayed Puberty
There is no fixed to start having periods, but if it does not starts by the age of 11, it is best to seek a doctor. Though many young girls start having a period at the age of 14 or so, lack of periods can also happen due to the absence of uterus, by birth. An expert gynecologist can verify the same and advice accordingly.
2. Menstrual Disorder
There can be several types of issues with the menstrual cycle. Heavy periods, scanty periods and irregular periods are most common. Mostly it can be addressed well with a healthy diet, active lifestyle and taking adequate rest in between. However, it is still best to keep track of it and seek consultation from a gynecologist.
3. White Discharge
Though white discharge is very common among women of childbearing age, it can be a bit heavy and troublesome for young girls. Maintaining proper hygiene is required, along with doctor’s advice, if needed.
4. Abnormal Facial Hair
During a young age, many young girls develop facial hair due to hormonal disbalance, which can be devastating for her self-image. Often it gets better with age, but still, it is wise to seek an expert opinion, cause many a time, it does require treatment to fix it.
Gynecological Problems During Adult Age
1. Infertility
The inability to have a successful natural conception or to carry a pregnancy is termed as infertility. Often it is due to some lifestyle factor such as smoking, overweight which can be resolved. However, infertility often occurs due to some more severe hormonal or gynecological conditions, which requires extensive fertility treatment from expert doctors.
2. PCOS
Polycystic Ovary Syndrome (PCOS) is one of the most common hormonal issues among women of childbearing age. It becomes more prominent and problematic during this phase. It starts to interfere with everyday life and other gynecological aspects of the body. Thankfully, it can be treated effectively with medication, lifestyle change, and surgery, if required.
Read more: 5 Facts About PCOS Every Women Should Be Aware Of
Gynecological Problems During Later Age
1. Menopause
It is the natural decline and eventually cessation of reproductive life. Though it is inevitable for every woman, it brings a hard time for many women, either physically, or emotionally, or both. It can be easily treated and thus, women should consider it if they feel they need help.
2. Gynecological Cancer
Gynecological cancers are yet another problem among older age grouped women. Cancer of Breasts & Uterus is more commonly diagnosed in older women as compared to the younger groups. Often it is due to aging and sadly, many a time, it is because of ignoring symptoms of the same for years. Either way, it should be treated form an expert gynecologist or oncologist at the earliest.
All the women are advised to keep track of their health routine, especially after attaining puberty. Availing well-women health check-up package once every 2-3 years is an excellent way of ensuring the same. Seek medical help if any alarming symptoms appear. Stay healthy, and always remember-
“There is a pain in being a woman, yes, but there is pride in it, too”.
-Mary Pauline Lowry
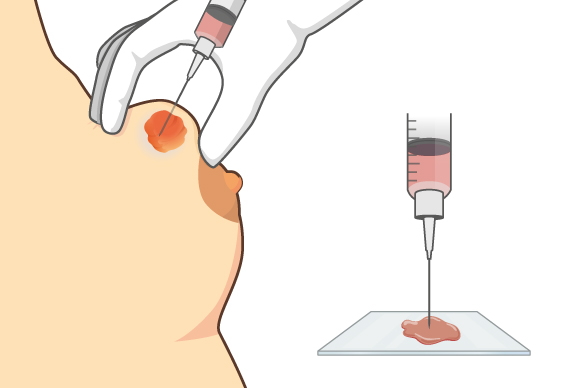
FNAC – How It Works And Helps Towards Detection Of Breast Cancer
Breast cancer is a leading cause of death among women all around the globe. The scenario is equally frightening in Indian as well. The detection of malignancy in the breasts happens in later stages in India, and that is why breast cancer treatment is not very effective for many women.
Timely screening can confirm whether or not it is a case of cancer and thereby, the suitable treatment can be pursued, if needed.
Gynecologists recommend that every woman above the age of 30 should pay attention to any changes that occur in their breasts. Let’s understand about one such crucial screening, the FNAC, in details.
What is FNAC?
FNAC stands for Fine Needle Aspiration Cytology. It is a diagnostic screening that can detect the malignancy in the breast tumor. It can also be used to aspirate a known cyst, by pricking and collecting fluid. It is done to remove the cyst completely or to relieve discomfort and pain that is quite common for large cysts.
How FNAC is carried out?
FNAC uses a thin needle to penetrate the breast tissue to reach the site of the tumor. The exact position of the cyst or tumor can be detected using ultrasonography and the needles are guided accordingly. It collects some cells or fluid as a sample. The sample collected is then sent to the laboratory to investigate its nature further.
This usually does not require any anesthesia, because even if the procedure requires pricking the breast with needles, the pain is bearable. However, it might require the same, if a solid system is concerned, which required multiple aspirations, in a single screening procedure.
How FNAC helps to detect breast cancer?
Prescribing an FNAC does NOT mean the doctor suspects breast cancer. In fact, mostly it is the opposite. Usually, when they come across any lump during a physical exam and suspect it to be a harmless, benign tumor, the first thing they recommend is the ultrasound and closely followed by FNAC.
The reason for recommending USG as foremost screening is simply to get the exact location of the lump. The FNAC test simply rules out the possibility of cancer. In case, it shows hints of malignancy, a biopsy is then recommended, which confirm the presence and type of malignancy.
So, why does the gynaecologist, does not recommend biopsy in the first go itself? Well, simply because FNAC is less invasive than a biopsy. A biopsy requires proper anesthesia as is a little more severe and sort of unnecessary for benign tumors.
What happens after FNAC confirms the nature of the tumor?
Well, if it shows malignancy, which is quite rare, the gynecologist is likely to refer the patient to an oncologist for advanced breast cancer treatment. In case its benign tumors, it can either be aspired to relived discomfort or left intact in the place (unless it projects any more trouble in the future) or it can be removed by surgery anyway.
For more information, if required it is wise to get in touch with a gynaecologist and discuss the possibilities.
5 Common Complications Faced By Pregnant Women
Carrying another life inside you is both a blessing as well as the most challenging task. Thankfully the expert gynecologist and obstetricians help you thoroughly for the same. In fact, maternity hospitals are all equipped to make this experience as comfortable and safe as possible. But there are certain complications that might make it difficult though. Here we present some complications that may arise during pregnancy.
1. Hypertension

It is also known as high blood pressure. It occurs when the blood flowing in the blood vessels exerts too much pressure. This happens when these vessels get narrowed due to some reason. This causes hindrance for the blood to reach the placenta (which provides oxygen and nutrition to the baby). This deprivation for long can cause a slower growth of the baby and can also uplift the chances of preterm labor.
2. Gestational Diabetes

It is a rather unique type of diabetes in which a pregnant woman, with no history of high blood sugar gets diagnosed with it. Even though most of the time gestational diabetes get resolves on its own, after childbirth, it uplifts the probability of several other complications during pregnancy and thus its constant treatment is required. Also, it makes the mother susceptible to diabetes in the future, so she should keep her sugar level in check.
3. Preeclampsia

It is a rather serious condition which has quite severe effects. Its causes are often unknown, but it can be a more likely scenario in case of the first pregnancy or in the case the mothers is obese or is older than 35, or carrying multiple babies or have suffered from the same condition in her previous pregnancy.
It is characterized by exceptionally high blood pressure and in case if it is left untreated it can cause organ damage.
4. Placenta Previa

As already discussed, placenta nourishes your baby before birth. The placenta is usually attached to the top of the uterus and in case of this complication, it slides down. It can cover the cervix (right on the birth canal) either partially or totally. Needless to say, it can cause a hindrance during childbirth and can make it strained labor for the mother and somewhat risky for the baby. It can be diagnosed accurately during a pre-natal scan. Extensive treatment under an expert obstetrician is crucial for such cases.
5. Severe Vomiting and Nausea

Morning sickness is quite common among expecting mother. It is characterized by feeling nausea and voting in the early morning, particularly during the first trimester. Its severe form is called hyperemesis gravidarum and it causes extreme nausea and vomiting along with weight loss, dehydration, fainting and loss of appetite that often need extensive treatment in some maternity hospital.
Good prenatal care is highly recommended for every pregnant woman along with timely medication and prenatal screening. It can ensure that any pregnancy-related complications can be addressed and treated effectively on time. Come at ILS Hospitals to have a safe pregnancy and childbirth ahead.
A Brief Introduction About Cervical Cancer Vaccination
Cervical cancer is the second most common form of cancer in women in India, after breast cancer. Cervical cancer refers to the malignancy found in the cervix (the lowermost portion of the uterus) of the reproduction system in women. Though cervical cancer affects older women of age 50 or above the most, many gynecologists confirm that women with the same have been diagnosed in their early 30s as well. Let’s understand regarding many of its aspects in details along with cervical cancer vaccination.
Cervical cancer might project no symptoms at first, but the advanced stages often show some symptoms such as vaginal discharge with blood or strong smell, bleeding in postmenopausal women or during times other than on periods, pelvic pain and so on. Though these symptoms might indicate some mild infections as well, it is always wise to get it checked to rule out the possibility of cervical cancer.
Cervical cancer occurs due to Human Papillomavirus Infection (HPI). It can be prevented effectively with the HPV vaccine. It usually takes 2 to 3 shots to complete the dosage. It is usually advised for young girls of age group 9-15, but can also be recommended to women reaching until the age of 25 or even more. A thorough consultation is advised to consider the same with an expert gynecologist, in depth.
Cervical cancer vaccination is not fully effective for women above the age of 25, particularly if they are already sexually active (It is true for even the younger girls). The reason being, the vaccination loses its effectiveness as women grow older, and moreover being engaged in sex, might already have exposed them to the infection, makes will make the vaccine considerably. However, the HPV vaccine can help prevent many other diseases of the reproductive tract as well.
Cervical cancer vaccination offers protection malignancy in the cervical region. But as HPV virus also can cause cancer in the vulva and vagina, this vaccination protects the women against these as well along with genital warts.
However, there are other measures that can help with early detection of cervical cancer too. Pap smear is a screening that collects sample cells from the cervical cavity. It is then evaluated under a microscope. In case they exhibit any changes in their structure, it might be indicating cancer and thus, timely treatment options can be availed for it.
HPV vaccination is effective and safe. The only side effects that have been found in some cases are pain, swelling, and redness in the site of the injection. However, these are mild and temporary and overall, its advantages surpass the mild discomfort.
ILS Hospitals offers HPV vaccination to fight cervical cancer effectively. We urge parents of every young girl to seek consultation with an experienced gynecologist to consider HPV vaccination for their daughters to have a cervical cancer-free life ahead. For women who are older are also advised to take proper measure to mitigate the possibility of cervical cancer in their future.
5 Useful Tips For A Healthy Motherhood Ahead
Mother is someone who holds us in her belly for 9 months, in her arms for three years and in her heart for a lifetime.
These few words are truest to its sense. Indeed there is no one like a mother. And today, we are going to offer a few useful tips as offered by leading gynecologists of ILS Hospitals, a renowned hospital in Kolkata, which will help you to have a safe pregnancy and childbirth ahead.
1. Reassure The Baby’s Heath
Get the primary test and prenatal scanning to ensure that your baby is doing good. Your prenatal scan tells much more about your pregnancy that you might realize. It reassures the pregnancy, number of babies you are expecting and a possible due date as well. Avail a baby scan from the best maternity hospital or a clinic with an expert gynecologist.
2. Eat Right At Right Time
Eating nutritious food is quite important during pregnancy. Not only you should be eating more, but you have to focus on consuming all the crucial nutrients as well. An expert gynecologist or obstetrician will guide you towards having an ideal diet chart for a healthy mother and child. Apart from a prenatal supplement, eat lots of fresh fruits and veggies, but remember to avoid the ones that are bad for your pregnancy (like papaya).
3. Stay Hydrated
You must be aware that pregnancy makes you ‘pee for two’. However, it is crucial that you drink for two as well. Staying hydrated will help keep your amniotic fluid in balance and also help you deal with nausea and morning sickness. Always keep a bottle of water you and keep taking sips every now and then. You can also consider having fresh juices and coconut water etc, to help intake more water.
4. Remove Few Things From Diet Chart
If you are engaged in bad habits like alcohol, smoking, etc, pregnancy might be the right motivation for you to quit it (and for your partner’s too). The harmful toxin of these, not only affect your health but your baby’s health as well. Moreover, try to limit the amount of caffeine you intake as well, as it too can cause some complication in your pregnancy.
5. Educate Yourself And Others
During pregnancy, you are never alone and you are not alone, going through it. So, consider joining a prenatal class. They offer several helpful tips on pregnancy, childbirth, nursing, and early parenting. Moreover, such help groups can offer assistance in more than one way.
We urge every budding mother and her family to take special care of her along with her baby’s. We, at ILS Hospitals, offer the best medical assistance and care for the expecting mother with our expert gynecologist and obstetricians. Moreover, we are also ready with neonatologist and pediatrician to take care of the infants, if they need it.
Hormonal Issues Faced By Women After Menopause
In this forever changing the world, ‘change’ is the only constant. It is particularly effective when aging is considered. Even though many illnesses keep surfacing through any age, some conditions strike due to aging. Menopause is one such condition that can cause many problems for women going through this stage. Menopause is the transition that marks the end of the reproductive age of a woman.
Today, we will talk about the hormonal issues faced by women after menopause and what needs to be done to address them, as per gynecologists.
There are two particular female hormones, namely estrogen and progesterone in the body. The overall balance and level of these hormones regulated and influence the menstrual cycle and fertility cycle. Their level decreases significantly during the menopause and as a result, it affects the overall health severely. For many women, these effects stay only for a short period of time and for many it stays effective for many years to come.
Symptoms Of Post-Menopausal Condition
Some of the most experienced symptoms of menopause are as follows-
- Irregular Periods Or Spotting
- Mood Swings Without Any Particular Reason
- Hot Flash Or Night Sweats
- Insomnia
- Tenderness And Lethargy
- Brain Fog And Feeling Out Of Focus
- Lack Of Interest In Intimacy
- Experiencing Pain Or Dryness In Intimate Regions
Many women become more susceptible to other conditions such as weight gain, osteoporosis, cardiac ailments, etc. However, the most severe effects often constrain in the mind and require long term medical care.
What Is To Be Done To Address It?
As per many studies, the emotional turmoil is more prevalent among women in western countries, as menopause is considered as a sign of aging. Thankfully, in southern Asian countries, like in India, not many women severely suffer (emotionally) due to menopause, as socially and physiologically, aging often is considered as a mark of wisdom. Though many women find this transition quite easy to deal with, gynecologists acknowledge this as a medical condition and advise to seek treatment in case one is struggling with any discomfort.
Our expert Gynecologist offers effective treatment to the women dealing with the postmenopausal syndrome. Often medication is adequate to deal with the physical symptoms, however, for the mental and behavioral ones, they can also recommend therapy. Moreover, as mentioned earlier that menopause brings many secondary conditions, as a likely scenario, so it is crucial for post-menopausal women to keep their overall health in check as well.
Check Out The Medical Condition When Hysterectomy Is Required
The human body, its organs, and the organ system is a complex creation of nature. Each organ has its own set of function and significance. However, due to many complications, it might become important to surgically remove either a part or the entire organ. The uterus is the internal organ that plays a crucial role in pregnancy and menstrual cycle of women. Surgical removal of the uterus is called hysterectomy. Expert gynecologist and obstetrician recommend a hysterectomy for various reasons. Let’s understand what conditions calls out for the need of a hysterectomy.
1. Heavy Menstrual Bleeding
Some women experience severe bleeding during the monthly cycles up to an extent that it starts affecting their daily life. In such cases, hysterectomy offers a permanent solution as post surgery, the menstrual cycle ceases to continue. However, often it is availed only by the women who no longer wish to have children.
2. Uterine Or Cervix Cancer
Any cancer is a deadly medical condition that requires effective treatment on time. For any cancer, surgical removal of the site of malignancy is the best treatment and the same holds true for the gynecological cancers as well.
3. Endometriosis
The uterus lining tissues sometime might grow outside the uterus and spread into nearby organs such as a fallopian tube or other pelvic or abdominal organs. A total hysterectomy is considered when other medical approaches fail to get any effective results.
4. Fibroids
Uterine tumors, even if benign in nature, cause many complications. Pain, bleeding, and anemia is some of them. They can be treated by a non-surgical approach in case they are quite small in size. However, it might require a hysterectomy to address larger fibroids.
5. Pelvic Inflammatory Disease
It is a bacterial infection affecting the female reproductive system which can be cured easily with over-the-counter drugs if detected at its earliest stages. However, failing to do so, can have drastic consequences as it spreads to the uterus and fallopian tubes and causes a long term, severe pain. Hysterectomy remains a feasible and permanent solution for the same.
A partial hysterectomy is a procedure in which only the uterus is removed while the cervix is left intact. In a total hysterectomy, the cervix is also removed (many a time, either or both ovaries and fallopian tubes are also removed) surgically. At ILS Hospitals, we offer laparoscopic hysterectomy for patients dealing with such severe medical conditions.